Prior to the 1990s, ‘health’ was understood as a domestic issue for national government regulation, one that was outside the scope of International Relations (IR) theory and practice. Today, health challenges feature prominently in global security discourse, affect bilateral and regional political relationships between states, and are recognised as some of the most important non-traditional security issues in IR (Heymann 2015, 1884). The rise to prominence of the ‘global health security regime’[1] is historically unprecedented (Fidler and Draeger 2006, 687), and was achieved through the framing of specific health problems as security threats, and the development of a strategy to improve global health security through the creation and proliferation of new international norms. The evolution of the ‘global health security regime’ illustrates the role that international norms can play in global security; the emergence and socialisation of the norm of responding to health threats as security threats has reshaped and expanded the global security agenda.
To demonstrate this, this essay will proceed in three sections: first, it will define the social constructivist approach which is essential to understanding how norms play a crucial role in constituting international society. Secondly, it will use the securitisation of infectious diseases to demonstrate how ideational changes can provide the ‘embedded condition for norm entrepreneurship’; in this instance, securitisation acted as an enabling condition for the emergence of the new norms of the ‘global health security regime’. Third, this essay will examine the process of the revision of the International Health Regulations (IHR), using the three-stage model for explaining the norm lifecycle; this will show how the conscious promotion of new norms can, under the right circumstances, lead to the embedding of new global security practices.
Social Constructivism
Social constructivists argue that the social world is constructed (through inter-subjective interactions) rather than discovered (Andrews 2012, 1); that social agents and structures constitute one another mutually (Wendt 1992, 411), and; that ideas are central to this process, so that the constitution and dynamics of a community (the international community in the context of IR) relies heavily upon factors such as shared-norms and shared-identity (McDonald 2013, 64).
According to social constructivists, the behaviour of states within the international system is regulated by two types of norms: ‘soft’ (purely conventional and non-binding) norms and ‘hard’ (binding) norms; otherwise known as ‘binding international laws’ (Davies et al. 2015, 10). Both types of norms are able to regulate states’ behaviour because states have been constituted by, and exist within, a social structure whereby they will naturally want to conform to what is socially accepted and expected of ‘good’ states (see Finnemore and Sikkink 1998). Therefore they should be reluctant to act in ways that cannot be legitimated by prevailing laws, rules or norms (Davies et al. 2015, 10). Wendt argues that once norms are constituted, they reinforce certain behaviours and discourage others (Wendt 1992, 411). Thus, an indication of the existence of a widely shared international norm is ‘the presence or absence of justification or condemnation in cases of non-compliance’ (Davies et al. 2015, 11).
The emergence of constructivism in the post-Cold War era heralded a broadening and deepening of IR by opening up intellectual and policy space for the consideration of threats of a non-military nature (Yuk-Ping and Thomas 2010, 447). This is evident in the landmark 1994 United Nation Development Report entitled New Dimensions of Human Security, which ‘established the initial parameters of the nascent fields of non-traditional security research that were emerging’ (Yuk-Ping and Thomas 2010, 447). Following the release of this report, the IR practitioner’s engagement with new questions became possible, such as: ‘how are order, power and identity related?’, or; ‘how are interests constructed and changed?’ (Walker 1997, 64-65). Health became linked with IR through this process of broadening and deepening the focus of IR as well as its underlying ontological assumptions. States remained the primary focus, but the role that non-state actors, including international organisations such as the World Health Organisation (WHO), played in the international system increasingly became part of discussions due to the power that they had to dramatically impact states and societies (Davies 2010, 13).
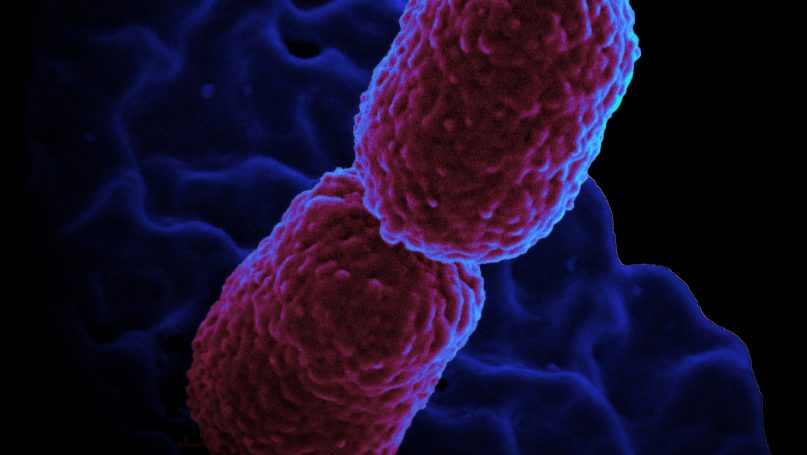
Securitisation of Infectious Disease
It is near impossible to understand the emergence of the norms associated with the global health security without taking into account the ‘crucial zeitgeist [surrounding] the securitisation of infectious disease’ that occurred in the 1990’s (Davies et al. 2015, 21).
Securitisation is a norm-establishing process whereby a non-security issue comes to be considered a security issue by international actors. In a framework put forward by the Copenhagen school of IR scholars that attempts to describe how securitisation works (see Buzan et al. 1998), it is proposed that for a threat to be identified as a security issue, the threat must first meet strictly defined criteria that distinguish it from a mere political issue (Buzan 1998, 21). A security issue then “has to be staged as an existential threat to a referent object by a securitising actor, [to generate] endorsement of emergency measures beyond the rules that would otherwise bind” (Buzan 1998, 21). Having met these criteria, the threat must then be accepted as a security threat by the securitising actor’s target audience (usually civil society.). In the final step of securitisation, the threat must generate extra-budgetary reallocation of resources to combat it. In the case of infectious diseases, securitisation elevated the status of the issue to the point whereby the impetus for resource reallocation and international attention was clear (McInnes 2004, 53-55).
Although, using the Copenhagen school’s framework, it is possible to gauge whether a threat has been successfully securitised or not, it should be noted that securitisation is not something that can be easily defined; “its meaning lies not in what people conceive its meaning to be, but how they implicitly use it… it is thus a self-referential practice” (Buzan 1998, 23). Society defines the limits on what can and cannot be securitized based on the perceived level of threat.
Regardless of how we define the process of securitisation, the value of securitising health issues, according to Enemark, is that it ‘promises to attract greater political resources and attention for protecting human health and human lives in the face of specific infectious disease threats’ (Enemark 2007, 20). The securitisation of global health, particularly regarding infectious disease outbreak events, means that states are more likely to take health threats seriously.
Indeed, the ‘securitisation’ phenomenon saw a dramatic increase in ‘security talk’ in national and international policy circles surrounding infectious disease following the end of the Cold War (Rushton 2014, 292). A burgeoning literature of IR and Political Science scholars concentrating on the relationship between heath and security emerged (some noteworthy contributions include; Enemark 2007; Fidler 2003; McInnes and Lee 2006; Price-Smith 2001, 2009). Along with this growing academic literature, policy workers also started writing about the relationship. An influential report by the United States’ Institute of Medicine in 1992 entitled Emerging Infections: Microbial Threats to Health in the US warned that the United States and the international community had ‘dropped the ball’ on international health and security. In the post-Cold War context, the US now had the capacity to listen to such an alternative security message (Fidler 1996, 79).
The process that securitising infectious disease threats has followed, and largely continues to follow, accords with Buzan’s framework. Under this framework, changes to the material circumstances of the international environment (e.g. the emergence of new diseases), or ideational developments within it (e.g. an increased focus on livestock as potential carriers of disease), can provide adequate stimulus for a new or existing infectious disease to be considered a security threat, or for a new norm to be developed surrounding the threat. However, even where such stimuli exist, it is how states perceive and respond to these changes in the international environment that ultimately leads (or does not lead) to the establishment of new norms (Davies et al. 2015, 12).
By the 1990s, ‘humanity had achieved a level of spatial, temporal and cognitive interconnectedness that had never before been witnessed’ (Kamradt-Scott 2015, 2); this phenomenon–globalisation–represented a material and an ideational change in the international environment. It created a new context within which infectious pandemics could take place; the human population grew, there was an unprecedented increase in the volume and pace of transnational movement, and a growing global inequality in terms of access to health care (Chen and Takemi 2015, 1887-1888). However, these factors alone did not lead to normative development, they had to be accompanied by changes in states’ perception of the threat of infectious disease, and ultimately consequential changes in behaviour. The treatment of infectious diseases as threats was the ideational backdrop and the security discourse became the embedding condition for norm emergence and eventually internalisation.
The Norm Lifecycle
The predominant account of how new international norms emerge and become embedded in state practice is Finnemore and Sikkink’s three stage model of the ‘norm lifecycle’ (Finnemore and Sikkink 1998, 896). To demonstrate how the norm evolution process can dramatically alter state practice in relation to global security, the three stage model can be used to track the development of the norm of securitising infectious disease threats.
By the late 1980s, it was clear that the existing IHR, adopted in 1969, were no longer ‘fit for purpose’: the WHO had no means of enforcing the IHR if a state was non-compliant with them, and was unable to act on information until an outbreak was formally reported and verified by the government themselves, which supplied a clear incentive to misreport (see IHR 1969). The IHR also failed to keep up with the emergence of new disease threats (e.g. HIV/AIDS), and limited their regulation to the traditional epidemics of: cholera, plague, yellow fever, smallpox, relapsing fever and typhus, due to historical precedence. In the context of increased international travel and trade, the IHR were clearly powerless to manage the emergent health threats that repeatedly threatened international systems.
In the first stage of the norm life cycle (‘emergence’) norm entrepreneurs seek to utilise the technique of persuasion to promote an incipient norm. At the 1995 World Health Assembly (WHA), political consensus emerged in the form of unanimous agreement over the need to revise the out-dated and ineffective 1969 IHR. Agreement was required to ensure that the WHO’s disease outbreak alert and response capabilities were appropriate for the current era. The power to revise the IHR that was vested in the WHO as a result of the WHA agreement provided the secretariat with a near perfect opportunity to engage in norm entrepreneurship to promote what they would label the ‘global health security regime’ (Davies et al. 2015, 27).
The norm entrepreneurs in this case were the WHO bureaucracy. In Barnett and Finnemore’s terms, the WHO had the ‘expert authority’ (Barnett and Finnemore 2004, 24-29) in its role as global medical technical agency, as well as a significant amount of ‘moral authority’ (Barnett and Finnemore 2004, 73). The WHO team tasked with the IHR revision process engaged in work to redefine what appropriate state behaviour during disease outbreak should look like, and to frame appropriate state behaviour in security terms, in order to gain political support and state buy in.
After informal consultation on the IHR revision process in 1995, the WHO released a first draft to its member states in 1998 (WHO 1998, 234). This was the first iteration of the new norms of global health security that the WHO promoted. At this stage, not all states were persuaded that the new norms provided an appropriate and effective solution to infectious disease control, or that they were compatible with some states’ existing normative commitments (i.e. the norm of sovereignty) (Davies et al. 2015, 41).
In the second stage of the norm life cycle (socialisation), once a critical mass of states adopt the new norm, it is said to reach a tipping point, following which a norm cascade begins. Finnemore and Sikkink state that socialisation is the ‘dominant mechanism of a norm cascade through which norm leaders persuade others to adhere’ (Finnemore and Sikkink 1998, 902). Despite the WHO secretariat agreeing unanimous in 1995 to the need to reform the IHR, by the late 1990s progress had reached a ‘virtual standstill’ (Kamradt-Scott 2010, 80). The ‘tipping point’ in this case was the Severe Acute Respiratory Syndrome (SARS) outbreak of 2003.
The SARS outbreak created a ‘sense of urgency’ that amplified the importance of the security framework promoted by the WHO (Davies et al. 2015 44). Indeed, the political fallout and human tragedy (with 8 400 infections worldwide and 774 deaths) (Heymann 2005, 16-17) of the crisis imparted a sense of urgency that had been lacking in the revision process (Whelan 2008). The impetus of that the SARS outbreak created helped cut through earlier indifference and opposition to the proposed IHR revisions. According to Finnemore and Sikkink, the real moment that categorises the ‘tipping point’ is when norm breakers become norm followers (Finnemore and Sikkink 1998, 902). The action of China during the SARS outbreak exemplifies this, in that prior to the disaster they were deliberately non-compliant and openly opposed to what they saw as the IHR revisions’ imposition on their sovereignty. Following the outbreak, in which China was severely affected both in terms of human and economic losses, the costs of non-compliance became clear to China and they became a norm promoter (Davies et al. 2015, 74). The Chinese government sought to mend their damaged international reputation and gain back the trust of the international community by demonstrating their compliance with the WHO’s recommendations (Price-Smith 2009, 145).
The official stated purpose and scope of the revised IHR according to the WHO is “to prevent, protect against, control and provide a public health response to the international spread of disease in ways that are commensurate with and restricted to public health risks, and which avoid unnecessary interference with international traffic and trade” (see IHR 2005). The regulations are no longer limited to specific diseases as was the case in the 1969 iteration, but are applicable to health risks, irrespective of their origin or source. States are required to strengthen core surveillance and response capacities (‘positive duties’[2]). Another significant change is that the WHO can now receive official reports of an outbreak from sources other than states.
The SARS outbreak showed how the new norms of collective security response was already socialised within the vast majority of states in the international system. The majority of states chose to comply with the WHO regulations during the outbreak, despite the lack of any formal obligation to do so at that time (Davies et al. 2015, 72). The SARS outbreak and aftermath showed that the norm entrepreneurs had successfully linked the new norms with states’ individual and collective security; “The ways which states interpreted the lessons from SARS–and the ways in which norm entrepreneurs used SARS to forward their case–led to a process of states gradually redefining their interests, a profoundly ideational shift” (Davies et al. 2015, 15).
In the third and final stage of the norm life cycle (‘internalisation’), the norm takes on a ‘taken for granted’ quality where compliance becomes automatic and routinized in domestic political arraignments and bureaucratic procedure. Internalisation of the new norms of global health security occurred with the formal adoption of the revised IHR by the WHA in 2005.
Following the SARS outbreak, states’ attitudes shifted from seeing the previous incarnation of the IHR as a set of rules that they may or may not comply with, to seeing them as a sensible set of regulations that they should comply with. This shift in attitudes was achieved by convincing states that not only was it their responsibility as a member of the international community, but also that it was very much in their self-interest to comply. This was formalised in the unanimously accepted IHR revisions in 2005.
Compliance and Capacity
Norm compliance is not only a question of willingness to comply with international norms, but, crucially, a question of having the material capacity to comply. The successful promotion of new norms that became embodied in the revised IHR was a necessary step in enhancing global health security, but was not, in itself, sufficient. When regulatory attempts such as the IHR impose positive duties on states, it must be supported by a commitment of financial and educational support for less developed nations, in order to ensure compliance.
As the recent Ebola outbreak in West Africa has demonstrated, the economic and political effect of infectious disease outbreaks can be catastrophic both in terms of lives lost and economic devastation. Other insecurities including conflict and poverty can heighten states’ and populations’ vulnerabilities to infectious epidemics, and cultural practices (such as burial rituals) can augment the impact of the epidemic (Chen and Takemi 2015, 1887). Shortcomings in technical and infrastructural ability to detect, report and contain outbreaks occurring in their territory hinders the ability of less developed nations to meet their IHR obligations, meaning that the compliance of less developed nations will continue to be low (Davies et al. 2015, 11-12). This is not necessarily an indicator of a lack of commitment to the norm on behalf of these states; often it is simply a matter of not having the necessary capacity to comply.
States’ Self Interest?
Price-Smith argues that IHR revision is a case of states rationally accepting measures that will protect their self-interest, rather than a commitment to collective security (Price-smith 2009). However, as Davies argues, it is only possible to understand why all states unanimously agreed to the onerous demands placed on them by the reform process if the importance of the ideational change that took place in the 1990’s is acknowledged (Davies et al. 2015, 15). That is, the burden placed on some states by the new IHRs, especially those who are less developed, is high, and compliance costly. It was the process of securitisation which effectively made the threat credible enough that such states were willing to adopt the changes, even though the economic cost for their developing economies was significantly different to those placed upon developed states.
A similar argument is put forward that ‘health’ is increasingly being deployed as a tool for achieving other ends in global politics, such as in foreign policy, foreign aid, or in warfare (Davies et al. 2014, 828). This has led to accusations of the co-option of the global health regime for self-interested purposes. However, even if it is the case that states compliance with new norms is based on self-interest, it does not negate the fact that the norms themselves have had a powerful influence in changing how states act and what is commonly understood as acceptable state behaviour.
One example of the role that norms have played in changing what is considered acceptable state behaviour in the space of global health security is the substantial increase in international diplomatic coordination around health, especially seen in response to recent global pandemics (e.g. HIV, SARS, H1N1) (Davies et al. 2014, 827). In policy, the 2008 UK white paper claimed ‘health is global’ and requires new forms of political as well as technical relationships to be developed (Davies et al. 2014, 827). The change is also seen in the way that key non-state actors such as the United Nations Security Council, the United Nations General Assembly, the World Bank, the G20 and the WHO have converged to tackle a growing number of global health issues, and have been flanked by a growing number of more recently established institutions set up to explicitly further that goal (for example UN Aids and the Gavi Vaccine Alliance) (Davies et al. 2014, 27-28). This new focus on global health is also evident in the post 2015 development agenda and the articulation of the new goals of global health governance.
Conclusion
The evolution of the global health security regime demonstrates the power norms have in reshaping and expanding the global security agenda through re-defining what is acceptable state behaviour. By capitalising on the securitisation of disease that occurred throughout the 1990’s, norm entrepreneurs effectively deployed a strategy for IHR revision. The SARS epidemic in 2003 acted as the tipping point for a ‘norm cascade’, leading to the internalisation of the new norms and the formal unanimous acceptance of IHR revision in 2005. Although norms have the potential to change state behaviour, acceptance of such new behavioural expectations does not automatically result in those expectation being filled in all cases, due to a lack of capacity or state self-interest. Despite this, the global health security regime remains influential and continues to be the dominant framework through which states deal with disease threats, a distinct shift from pre 2005 state approaches, which demonstrates the power of the role that international norms can play in setting the global security agenda.
References
Andrews, Tom. 2012. “What is Social Constructivism?” Grounded Theory Review (1:11).
Barnett, Michael and Finnemore, Martha. 2004. Rules for the World: International Organisations in Global Politics (Ithaca: Cornell University Press).
Bull, Hedley. 1977. The anarchical society: A study of order in world politics. (Columbia University Press: New York).
Buzan, Barry. 1998. ‘Security Analysis: Conceptual Apparatus’ in (eds. Buzan, Barry., de Wilde, Jaap and Wæver, Ole) Security: A New Framework for Analysis. (Lynne-Rienner: Boulder) 21-47.
Buzan, Barry., de Wilde, Jaap and Wæver, Ole. 1998. Security: A New Framework for Analysis. (Lynne-Rienner: Boulder).
Chen, Lincoln and Takemi, Keizo. 2015. “Ebola: Lessons in Human Security” in (eds. Heymann, David L., Lincoln Chen, Keizo Takemi, David P. Fidler, Jordan W. Tappero, Mathew J. Thomas, Thomas A. Kenyon, et al.) Global health security: The wider lessons from the west african ebola virus disease epidemic. (Lancet: England) 385 (9980): 1887-1889.
Committee on Emerging Microbial Threats to Health, Institute of Medicine, Committee on Emerging Microbial Threats to Health, and Institute of Medicine (U.S.). 1992. Emerging infections: Microbial threats to health in the united states. (National Academies Press” Washington DC).
Davies, Sara., Kamradt-Scott, Adam and Rushton, Simon. 2015. Disease Diplomacy: International Norms and Global Health Security. (John Hopkins University Press: Baltimore).
Davies, Sara. 2010. Global Politics of Health (Cambridge MA: Polity Press).
Davies, Sara., Elbe, Stefan., Howel, Alison. and McInnes, Colin. 2014. “Global Health in International Relations: Editors’ Introduction” Review of International Studies 40: 825-834.
Enemark, Christian. 2007. Disease and Security: Natural Plagues and Biological Weapons in East Asia (London: Routledge)
Fidler, D. 1996. “Globalisation, International Law” Emerging Infectious Diseases 2:77-84.
Fidler, David. 2003. “Public Health and National Security in the Global Age: Infectious Diseases, Bioterrorism and Realpolitik.” George Washington International Law Review 35: 787-856.
Fidler, DP and Draeger N. 2006. “Health and foreign policy.” Bulletin of the World Health Organization 84: 687.
Finnemore, M. and Sikkink, K. 1998. “International Norm Dynamics and Political Change.” International Organisation 54:2, 887914.
Heymann, David. 2015. “The True Scope of Health Security” in (eds. Heymann, David L., Lincoln Chen, Keizo Takemi, David P. Fidler, Jordan W. Tappero, Mathew J. Thomas, Thomas A. Kenyon, et al.) Global health security: The wider lessons from the west African Ebola virus disease epidemic. (Lancet: England) 385 (9980): 1884 – 1886.
Heymann, David L., Lincoln Chen, Keizo Takemi, David P. Fidler, Jordan W. Tappero, Mathew J. Thomas, Thomas A. Kenyon, et al. 2015. Global Health Security: The Wider Lessons from the West African Ebola Virus Disease Epidemic. (Lancet: England) 385 (9980): 884-901.
Heymann, David. 2005. “SARS: A Global Perspective” in Severe Acute Respiratory Syndrome: ed. Malik Peiris, Larry J. Anderson, Albert Osterhaus, Klaus Stohr and Kwok’yung Yuen. (Malden, MA: Blackwell Publishing) 13-20.
International Health Regulations. 1969. WHO (Online) (Available): http://www.who.int/csr/ihr/ihr1969.pdf
International Health Regulations. 2005. WHO (Online) (Available): http://www.who.int/ihr/9789241596664/en/
Kamradt-Scott. 2010. “The WHO Secretariat, Norm Entrepreneurship, and Global Disease Outbreak Control”. International Organisation Studies 1: 72-89.
Kamradt-Scott. 2015. Managing Global Health Security: The World Health Organisation and Disease Outbreak Control (Palgrave McMillian: UK).
McDonald, Matt. 2013. “Constructivisms” in (ed. Williams, Paul) Security Studies: An Introduction. 2nd Edition (Routledge: New York).
McInnes, Colin and Lee, Kelly. 2006. “Health, Security and Foreign Policy.” Review of International Studies 32:5-23.
McInnes, Colin. 2004. “Health and Foreign Policy” in (ed. Ingram, Alan) Health, Foreign Policy and Security: Towards a conceptual Framework for Research and Policy (Nuffiend Trust: London).
Price-Smith, Andrew. 2001. The Health of Nations: Infectious Disease, Environmental Change and Their Effects on National Security and Development (Cambridge MA: MIT Press).
Price-Smith, Andrew. 2009. Contagion and Chaos: Disease, Ecology and National Security in the Era of Globalisation (Cambridge MA: MIT Press).
Rushton, Simon. 2014. “Arguments for Securitizing Global Health Priorities” in (Brownn, G., Yamey, G. and Wamala, Sarah) The Handbook of Global Health Policy (John Wiley and Sons: UK).
United Nations Development Report. 1994. New Dimensions of Human Security (Online) (Available): http://hdr.undp.org/en/content/human-development-report-1994
Walker, R.B.J. 1997. “The Subject of Scrutiny” in (eds. Krause, Keith and Williams, Michael) Critical Security Studies: Concepts and Cases (ULC Press: London).
Wendt, Alexander. 1992. “Anarchy is what States Make of It: The Social Construction of Power Politics.” International Organisation 46: 391-425.
Whelan, M. 2008. Negotiating the International Health Regulations. Global Health Working Paper No. 1. (Graduate Institute: Geneva)
WHO. 1998. “Revision of the International Health Regulations: Progress Report, July 1998.” Weekly Epidemiological Record 73: 233-240.
Yuk-Ping, Catherine and Thomas, Nicholas. 2010. “How is Health a Security Issue? Politics, Responses and Issues.” Health Policy and Planning 25: 447-453.
Endnotes
[1] ‘Global health security regime’ is defined as the behaviour expected of states and other actors in the event of a disease outbreak of international significance as stipulated in the International Health Regulations 2005
[2] ‘Positive Duties’ oblige states to take action, whereas ‘negative duties’ require states to only abstain from certain actions.
Written by: Josie Hornung
Written at: The Australian National University
Written for: Dr Cecilia Jacob
Date written: October 2015
Further Reading on E-International Relations
- Risk Theory vs. Securitisation: An Analysis of the Global Surveillance Program
- High North – Low Tension? Norway, Russia and Securitisation in the Arctic
- The Absence of Methodology in Securitisation Theory
- Securitisation, China and FDI: The EU’s Foreign Direct Investment Screening Regulation
- The Non-Politics of the Responsibility to Protect Through a Securitisation Lens
- Humanitarianism and Securitisation: Contradictions in State Responses to Migration