Fear of Ebola continues to grow around the world as the outbreak in Sierra Leone, Guinea, and Liberia worsens and new cases are confirmed in the US and Europe. Ebola is a contemporary health crisis in that it threatens the lives of many living in these three countries, has the potential to destabilise the economies of West Africa, and breeds feelings of insecurity throughout the region and the globe. This article argues that Ebola is not just a health crisis but represents a crisis of the health institutions and governance mechanisms that are supposed to contain such problems. Problems with institutions of global health have been discussed at length in studies on global health governance (see, for example, Youde, 2012; Global Health Watch, 2011), particularly with reference to WHO (Clift, 2013). Ebola brings the problems of global health governance starkly into view. The article makes this argument by first outlining why Ebola came to be a crisis and how global health priorities and the last fifteen years of health financing have led to neglect of the very health systems that are struggling to cope with the disease. Second, the article reviews the wider problem of competition and lack of leadership in global health governance that has inhibited the global response to the crisis. Finally, the article reflects on what Ebola tells us about global health governance and politics of a health crisis.
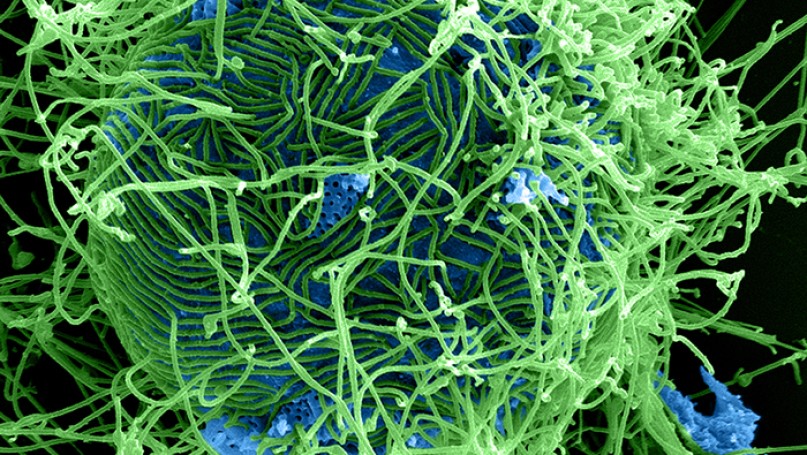
Incidents of Ebola are not uncommon. However, they tend to be rare and contained. The current outbreak of Ebola is a crisis because of the rapidity in which it has spread in Guinea, Sierra Leone, and Liberia, and the notion that the global health community has failed to bring it under control. Ebola is not an airborne disease and, while infectious, is only transmitted human-to-human through contact with bodily fluids (WHO, 2014). Hence, if appropriate precautions are taken, it can be contained and the rate of transmission should be low. However, this relies on effective and fully functioning health and education systems that can inform populations as to how to avoid transmission, and provide appropriate care and treatment for people showing symptoms of Ebola and those that provide care. As with any health intervention, this requires trust between the people and the services that are delivering care or health communication, be that the government or local health worker. The problem with the current crisis in West Africa is that health systems in these countries were ill-equipped and ill-staffed to respond to the crisis, there was a breakdown of trust and information between the public and the government, and there was a lack of international support to mobilise a wide-scale and rapid response.
On the one hand, why the health systems of these countries have been unable to cope with Ebola can be explained by a lack of government investment in public health infrastructure or health surveillance structures to identify and contain the spread of new diseases. However, such an explanation rests on the presumption that strategic planning and financing for health in West African countries is done by the government alone, rather than a myriad of intergovernmental organisations, bilateral aid agencies, and non-governmental organisations. Each of the three countries affected by Ebola is an aid recipient country and, as a consequence, embedded within the wider norms and priorities of global health institutions. Over the last ten years, these health priorities have been organised around the three health goals of the UN Millennium Development Goals (MDGs): Goal 4, Reduce Child Mortality; Goal 5, Improve Maternal Health; and Goal 6, Combat HIV/AIDS, Malaria, and other diseases (UN, 2014). Guinea, Liberia, and Sierra Leone have sets of indicators and targets tied to meeting these goals (UNDP, 2013).
The impact of the MDGs on health planning and spending has been significant. First, they have generated a considerable amount of finance, effort, and new institutions towards meeting the goals. This is particularly the case of HIV/AIDS that has generated an unprecedented level of commitment from a wide range of public, private, local, regional, national, and international bodies. The upsurge in money and institutional interest in HIV/AIDS has led to a distortion in many health systems in Africa where the health system is organised around HIV/AIDS programmes, because of the money available from new funding mechanisms, such as the Global Fund to Fight AIDS, Tuberculosis and Malaria (Harman 2012). Second, the identification of three specific health goals and the funding that has accompanied them has generated health silos where vertical or disease-specific interventions have been prioritised over horizontal interventions that fund the health system more broadly. Health silos result in the clustering of funds towards specific diseases, under-funding towards other health concerns, and competition between different branches of the health system over their-specific intervention (Harman 2012). Finally, the MDGs have created a results-based culture that is guided by investing in what can easily be measured – for example, number of children that have received a Polio vaccination – rather than the complexity of health systems that cannot easily be quantified. The consequence of these three factors is that health systems – hospitals and clinics, procurement structures, clinical professionals, ICT, equipment and supplies – have been neglected. Such neglect is starkly revealed when countries have to respond to a health crisis like Ebola. While money towards health concerns in Africa grew significantly since the millennium, with many suggesting a ‘golden age’ of global health, it is clear that a narrow focus on goals, targets, and performance missed what is core to the health of any population: a functioning health system.
The lack of attention towards health systems reveals a wider problem with global health governance: competition, confusion, and a lack of leadership. The World Health Organisation (WHO) has long argued for the need for investment in health systems, yet it has been hamstrung to act in this area because of its diminished role in global health governance and lack of resources. As the principle UN agency for health, the WHO should occupy a central role in global health governance. However, as a result of internal tensions and an external perception problem that it lacks dynamism and an ability to act, the WHO has been hollowed-out with regard to how it is financed, cuts in staff, and competition from other institutions. New institutions – such as the Joint United Nations Programme on HIV/AIDS (UNAIDS); the Global Fund to Fight AIDS, Tuberculosis and Malaria; and GAVI – have all been created outside of WHO to act on a range of specific disease interventions. These institutions have undermined the mandate of WHO, distorted funds away from the institution, and led to confusion and competition when acting in-country as to who is responsible for what (Harman 2012). In addition to the new institutions, older institutions, such as the World Bank and the United Nations Children’s Fund (UNICEF), are also engaged in the global health space. If you then add in multiple non-governmental organisations, private philanthropy such as the Bill and Melinda Gates Foundation, bilateral donors, and private actors such as pharmaceutical companies the landscape of global health governance becomes even more blurred. The result of which is lots of actors committed to global health, but no leadership as to how such institutions could work together (Harman and Rushton 2014).
The lack of leadership, initiative, and collaboration among global health institutions can be clearly seen in the current response to Ebola (Gostin and Friedman, 2014). The global response to Ebola has been delayed, with attention towards the outbreak in West Africa only gaining momentum once the first cases of the disease were identified in the US and Europe. In October 2014, World Bank President Jim Kim acknowledged the global response was coming too late and that the Bank had argued with WHO over the response (Elliott, 2014). Funding and personnel support to help stem Ebola in West Africa has been predominantly bilateral, with states giving to specific countries and financing specific areas, rather than contributing money to the global funding facility. As of October 2014, only $100,000 of the $1 billion required had been contributed to the UN’s Ebola Fund (Nichols and Wroughton, 2014), and the sending of medical personnel remains contentious. Europe and the US have divided-up responsibility along old colonial ties and strategic interests, with the UK taking a lead in Sierra Leone, the US in Liberia, and France in Guinea. Thus, what we can see is a familiar pattern to global health governance: bilateral and earmarked financing over multilateral processes, a weakened WHO, and a lack of leadership in motivating and co-ordinating the international community to effectively respond to a very real health crisis.
Ebola reveals the following about the politics of a health crisis. First, the globality of global health governance is a fallacy. Global co-ordination and collaboration among institutions and states is difficult to achieve and, in practice, becomes the exception rather than the norm. The response to Ebola is indicative of international rather than global health governance. Second, institutions of global health are unable to respond to global health emergencies, particularly when they impact on regions of the world that are not seen as strategically significant by the rest of the world. A very real health crisis in West Africa becomes a global health emergency when it affects the US and Europe. Third, global health institutions have long ignored the basic needs of health provision – health systems – and encouraged countries to prioritise vertical health interventions. In doing so, they have undermined the ability for states in low and middle income countries to respond to new or emergent health issues that are not an existing priority on the global health agenda. Health ministers of African countries have known this for a long time. Ebola is not only a health crisis for the people, society, and economies of West Africa; it is a crisis of divisive global health governance.
References
Clift, Charles. (2013) The Role of the World Health Organization in the International System. London: Chatham House, Working Group on Governance: Paper 1.
Elliott, Larry. (2014) ‘Ebola crisis: global response has ‘failed miserably’ says World Bank chief’, The Guardian, 9th October 2014, (accessed October 2014).
Gostin, Lawrence O. and Friedman, Eric A. (2014) ‘Ebola: a crisis in global health leadership’ The Lancet 384 (9951), pp. 1323 – 1325.
Global Health Watch (2011) Global Health Watch 3 London: Zed Books.
Harman, Sophie. (2012) Global Health Governance Abdingdon: Routledge
Harman, Sophie and Rushton, Simon. (2014) ‘Analysing Leadership in Global Health Governance’, Global Health Governance, Fall 2013.
Nichols, Michelle and Wroughton, Lesley. (2014) ‘UN Ebola Trust Fund gets $100,000, almost $1 billion needed’, Reuters UK, 17th October 2014, (accessed October 2014).
WHO. (2014) ‘Factsheet on Ebola’ (accessed October 2014).
UN. (2014) ‘The Millennium Development Goals’ (accessed October 2014).
UNDP. (2013) ‘MDG Progress Reports – Africa’ (accessed October 2014).
Youde, Jeremy. (2012) Global Health Governance. Cambridge: Polity.
Further Reading on E-International Relations
- American Global Health Internationalism and the Ebola Crisis in West Africa
- Ebola Response in the Democratic Republic of Congo: A Bridge to Peace?
- The EU’s Global Health Crisis Management: Past and Present
- Containing Coronavirus: Resilience in Times of Catastrophe
- What International Relations Tells Us about COVID-19
- Opinion – How Global Politics Exploits Women’s Health