
This excerpt, from Achille Mbembe, a Cameroonian author, refers to the current moment shared by the whole world and all its inhabitants: “As what is both off the ground and our common ground, the universal right to breath is not quantifiable. It cannot be appropriable. It is a right in relation to the universality not only of each member of the human species, but of the living as a whole. It must, therefore, be understood as a fundamental right to existence. As such, it cannot be subject to confiscation, and escapes all sovereignty in itself. It is, moreover, an original right to inhabit the Earth, proper to the universal community of its inhabitants, humans and not humans” (Mbembe, 2020). The year 2020 saw the advancement of a disease, which is believed to have started in China and later spread across the globe from major centers, the main power poles in the world. In this way, the dangers for humanity have become more latent. This statement, however, does not refer only to the spread of the disease. These dangers are more and more existential, with greater risk for and making the life of the marginalized strata of society unfeasible, such as Africans and refugees, among others.
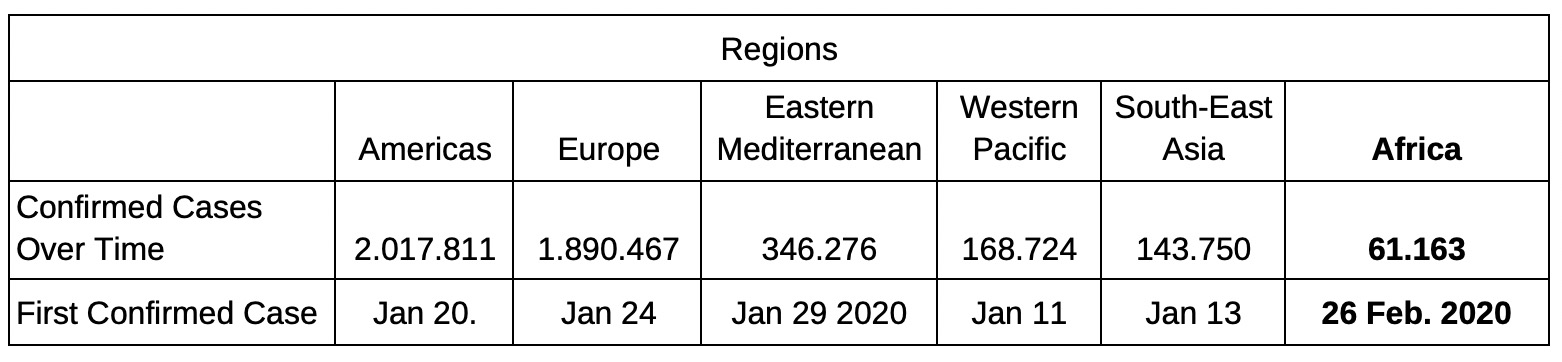
This discussion on the COVID-19 pandemic will be guided by the following question: Does the COVID-19 pandemic affect everyone in the same way? We depart from the reflection of a society that is already asphyxiated, beyond the biological aspects that are afflicted by the virus. Thus, 2020 received COVID-19, an infectious disease caused by the new coronavirus that causes respiratory problems and requires special treatment. Elderly people and/or those with pre-existing diseases – such as vascular or respiratory problems, diabetes, and cancer – have greater chances of developing the disease more severely. Its transmission occurs mostly through saliva or nasal discharge from infected people when coughing or sneezing. Declared a pandemic by the World Health Organization (WHO) on March 11, 2020, COVID-19 has already infected 4.628.903 people, resulting in the death of 312.009 of them, with an average lethality rate of 6.74% (data from May 15, 2020)[1]. The cases have been reported in 216 countries, regionally allocated according to the table below. It is worth mentioning that we consider the WHO’s criterion of an African region, which considers Africa the south of the Sahara, disregarding the countries of the north and the east – the so-called Horn of Africa.
WHO data from 18 May 2020.
The first cases of COVID-19 occurred in December 2019, in China. The country reported cases of severe pneumonia by unidentified agents. Chinese authorities identified and isolated the new type of coronavirus in January 2020. In January 2020, cases were reported in Thailand, Korea, and Japan, spreading across Asia and reaching Europe and the United States (USA) later that month, according to the first WHO report. It should be noted that the spread occurred from the central areas to the peripheral regions and that the first epicenters of the disease occurred in the largest production centers in their respective areas – such as Beijing, Milan, Paris, London, and New York. The acceleration of contagion in these areas was made possible, above all, because of air transport mobility inherent to the globalized world, and the spatial organization structure presented by agglomerations, mainly in large cities.
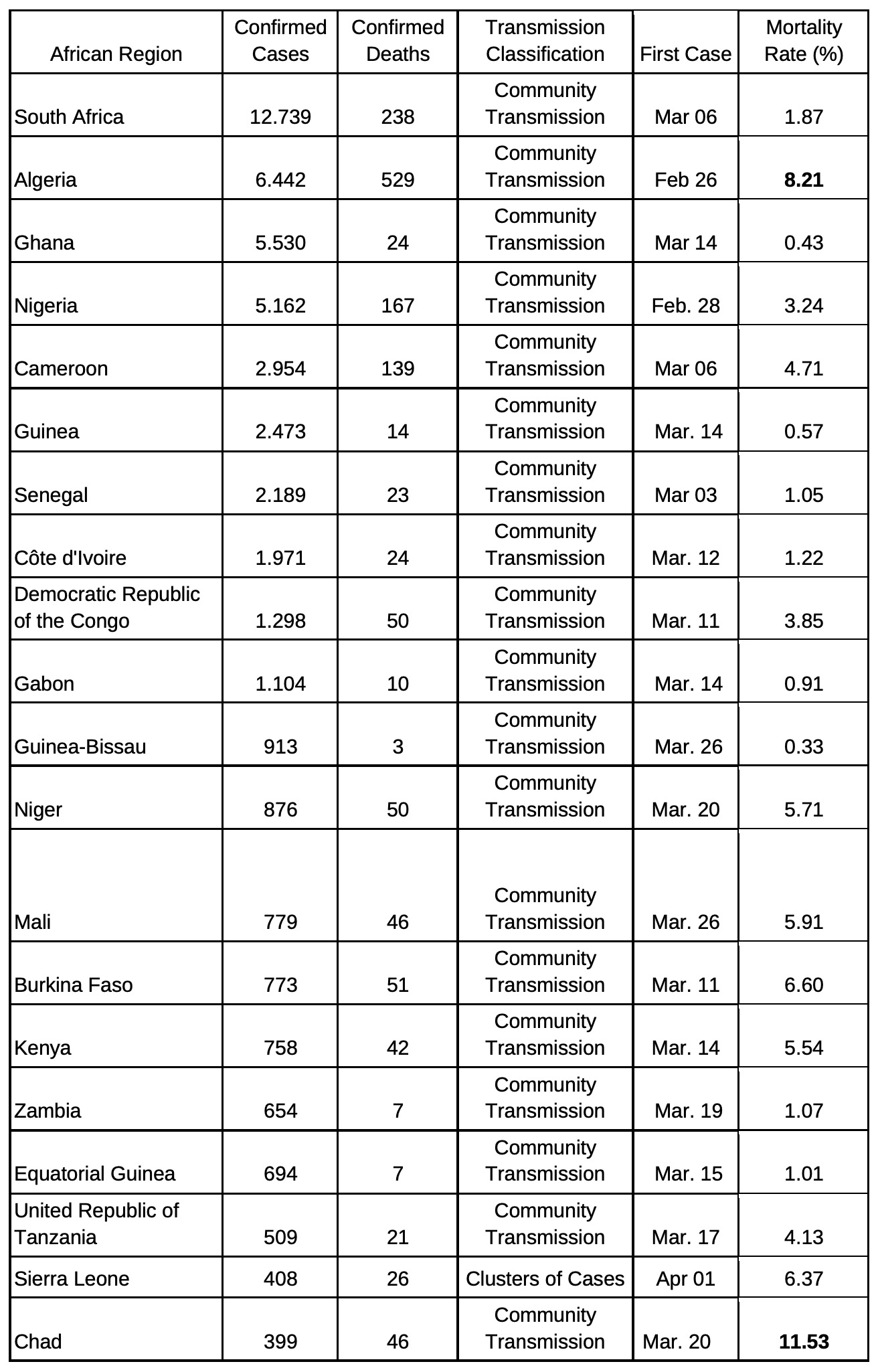
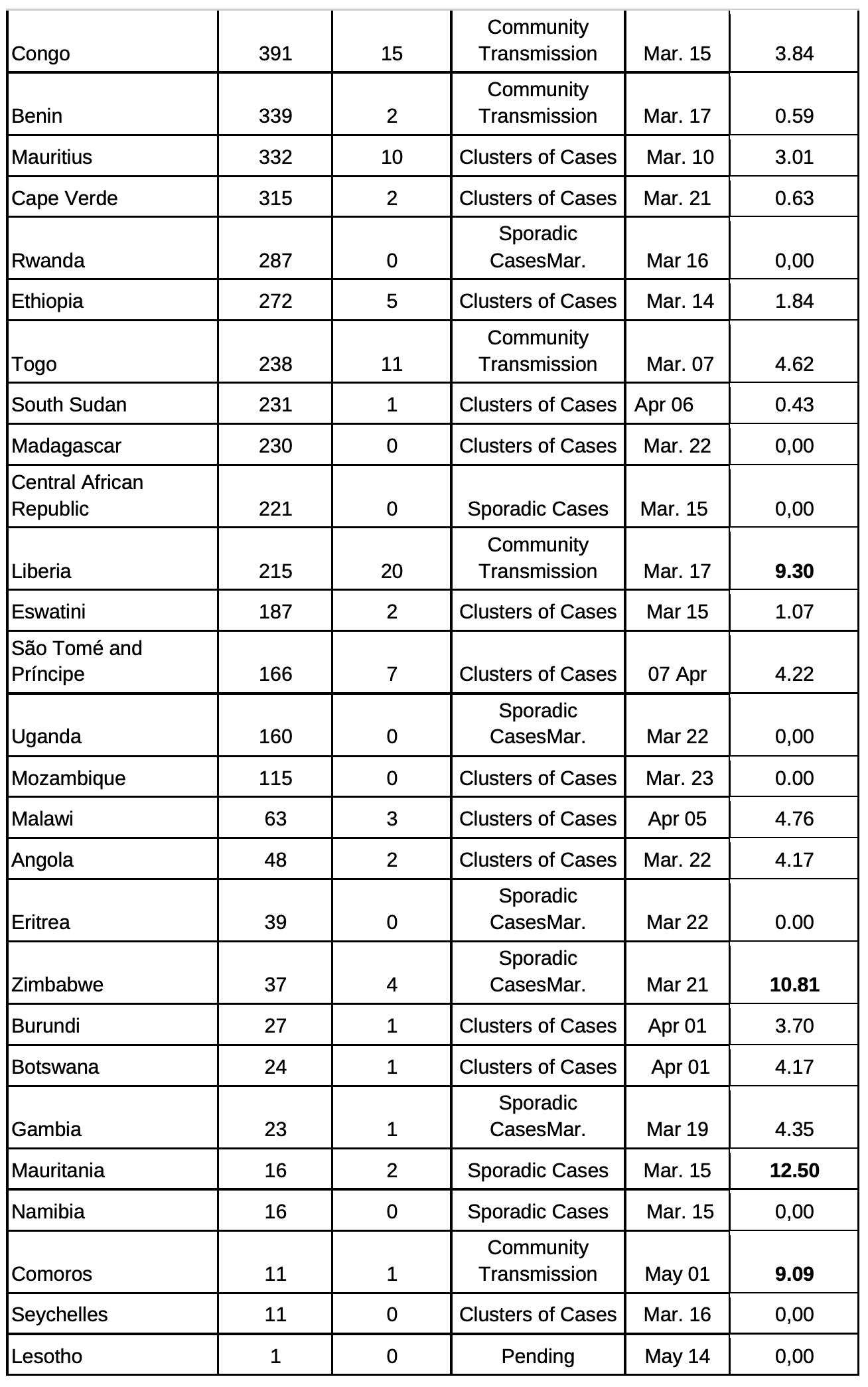
According to the table below the first reported cases in Africa were in Algeria and Nigeria, on February 26, 2020, and February 28, 2020, respectively, followed by Senegal (March 03, 2020), Cameroon, and South Africa (both on March 06, 2020). It is worth noting that these countries have strong relations with the outside world, especially with China, thus resulting in imported cases of citizens returning from travels. In southern Africa, for example, Johannesburg’s airport in South Africa was the main gateway for the virus, via Beijing.
Data of COVID-19 infections by countries in the African region: WHO data until 15 May 2020. Emphasis on countries with a lethality rate above the world average of 6.74%.
 Thus, similar to other epidemics, such as SARS (2002–2003) and H1N1 (2009), COVID-19 arrived last on the African continent. Gómez Díaz and Cruz Mata (2020) present other emergencies that African countries still face is relevant and are concurrently occurring with COVID-19. We can highlight, as an example, the fight against diseases such as measles, malaria, AIDS, tuberculosis, other tropical diseases, and isolated cases of Ebola – the outbreak occurred between 2014 and 2016 causing the death of 11.310 people in this period. Despite this last outbreak, there have been sporadic cases of Ebola since 1976, which persists. Ebola’s case presents some reflections that can be used in parallel to think about COVID-19 in Africa. During the mentioned period of the outbreak, the mortality rate was 40%, reaching 67% in 2019 in the Democratic Republic of Congo (DRC). However, in cases exported to First World regions – USA and Europe, with more advanced health systems – the lethality rate decreased to 27.8%.
Thus, similar to other epidemics, such as SARS (2002–2003) and H1N1 (2009), COVID-19 arrived last on the African continent. Gómez Díaz and Cruz Mata (2020) present other emergencies that African countries still face is relevant and are concurrently occurring with COVID-19. We can highlight, as an example, the fight against diseases such as measles, malaria, AIDS, tuberculosis, other tropical diseases, and isolated cases of Ebola – the outbreak occurred between 2014 and 2016 causing the death of 11.310 people in this period. Despite this last outbreak, there have been sporadic cases of Ebola since 1976, which persists. Ebola’s case presents some reflections that can be used in parallel to think about COVID-19 in Africa. During the mentioned period of the outbreak, the mortality rate was 40%, reaching 67% in 2019 in the Democratic Republic of Congo (DRC). However, in cases exported to First World regions – USA and Europe, with more advanced health systems – the lethality rate decreased to 27.8%.
Given these rates, we can see the differences between North and South, producing the existing borders. This is not only about the borders in the geopolitical sense, but the boundaries established in the social field, putting the value of life into perspective to understand one life as more valuable or important than the other. As a recent example, we have the supposed proposal of French scientists to test a possible vaccine against COVID-19 in Africans. This proposal provoked the reaction of several African people, including athletes and organizations like the African Union (UN), with the slogan “Africans are not lab rats”. This claim is supported by the Mbembe assumption in which the African people, since colonization, was “transformed” into a commodity by Europeans, who began to outline the guidelines and paths to be followed by them.
We can see, then, that the diseases mentioned, despite presenting great challenges, are not the only ones to be faced in the continent. The fragility of the health system, with few material and human resources, presents itself as one of the main obstacles to coping with epidemics or the COVID-19 pandemic. In addition to the precariousness of public health in sub-Saharan Africa, there are statistical problems since a large part of the population does not have access to the already scarce health systems, which can result in a high rate of cases underreporting.
It should be noted that, according to the statistical data presented here about COVID-19, some countries have a lethality rate that is much higher than the world average. The reasons for this are multiple. The first possibility is a high mortality rate by COVID-19 due to the precarious nature of African health systems, in line with other problems on the continent. There is, however, a second possibility: lethality may not be consistent with the data presented due to the great underreporting because of the previously mentioned problems. If the second hypothesis is occurring, the measures outlined to face the pandemic will be at risk, since the number of infected people and that should be isolated will be very different from the reality presented by the incomplete data.
However, we can see the complexity among the countries of the region. While some countries have high mortality rates due to COVID-19, in others this rate is zero. This is mainly due to the coping measures adopted by each country. While Rwanda took drastic measures when there were only 20 cases, Tanzania did not take any measures, with speeches urging the population to resort to magical or miraculous powers. It is noteworthy that WHO’s studies point to a continental catastrophe, with around 83.000 to 190.000 dead and 29 million to 44 million infected if measures such as social isolation and improvement of health systems are not adopted.
These problems are compounded by another the African issue: the refugee crisis. The continent has a large number of refugees and displaced persons who are located in overcrowded camps. It is worth noting that, according to UNHCR, West and Central Africa are home to large numbers of refugees, most of them from neighboring countries in the region. It is worth mentioning that in the camps that shelter the refugees there is difficulty in accessing sanitary resources and drinking water, hindering the hygiene measures necessary to face the coronavirus. Another difficulty in these fields is food shortage making these populations weaker, therefore, more susceptible to getting seriously ill. It is worth remembering that the basic needs of this population depend on international and non-governmental organizations.
We cannot forget, however, the economic impacts that will result from this pandemic and will affect the whole world. These consequences could impact Africa more drastically because of its economic vulnerability and its heavy dependence on the informal economy. Thus, the AU points out that the continent can be affected by two types of factors: exogenous and endogenous. The first is related to the decline in tourism, of foreign direct investment (FDI), and the reductions in trade with developed countries, which will have less demand for African products, namely commodities. This will have endogenous impacts. With a reduced demand, commodity prices will fall, reducing the collection by governments. In addition, there will be an increase in spending by these governments aimed to combating the pandemic.
Furthermore, we must consider another African characteristic: its strong dependence on the informal economy. The impact of COVID-19 will occur in two ways in this sector. The first impact is the economic one, similar to the impacts on the formal economy since a large part of the informal economy occurs in mining. The fall in demand will lead to a drop in the prices of these minerals. The second point to be considered is similar to the issue of refugee camps. In these mining areas, in addition to overcrowding, people have little access to hygiene and health conditions. Also, they are invisible to the local government, remaining dependent on non-state armed groups.
Besides, it is necessary to reflect on the late character of the arrival of COVID-19 in the African region, which may still be in its growth phase, since some countries have not registered community transmission so far. It must be taken into account the lack of resources and the low number of tests, which can result in great underreporting of cases, on top of the health and food problems faced by the population, making them more susceptible to the spread of the virus. It is also worth remembering that, with the comparison with other epidemics, the continent is seen as qualified to seek answers to the crisis, using, for example, the facilities used in the Ebola epidemic to confront the COVID-19, as in the DRC. Also, Senegal seeks to produce kits for low-cost fast-testing, and South Africa is testing the efficacy of the tuberculosis vaccine (Bacille Calmette-Guerin – BCG) against COVID-19. This raises the question whether the continent would be able to adapt quickly to this new major crisis in order to avoid a catastrophe of continental proportions in terms of statistics.
The African continent, facing its vulnerabilities, presented here, suffers a greater impact in face of the consequences of the COVID-19 pandemic, because amid the pandemic other social issues are pressing and require attention. Besides, the proposal of the French scientists points to the belief that the North gives itself the right to decree who lives or who dies, or how marginalized populations should live. Therefore, given the above, we realize that the virus does not affect everyone equally and the pandemic intensifies the existing lines of social segmentation.
Note
[1] It is important to explain that until the end of this work, these data were in an ascending curve.
References
African Union. Impact of the Coronavirus Covid-19 on the African Economy. Adis Abeba: African Union, 2020.
Gómez Díaz Elena; CRUZ MATA Israel. Por qué preocupa tanto la pandemia de COVID-19 en África. The Conversation España, Madri, 01.04.2020.
Mbembe, Achille. O direito universal a respiração. Texto (020). São Paulo: n1edições, 2020.
United Nations High Commissioner For Refugees (UNHCR). Global Trends: Forced Displacement in 2018. Disponível em: https://www.unhcr.org/globaltrends2018/
World Health Organization (WHO). Novel Coronavirus (2019-nCoV) Situation Report – 1 – January 21, 2020 – Disponível em: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4
World Health Organization (WHO). Coronavirus disease (COVID-19) Situation Report – 116 – May 15, 2020. Disponível em: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200515-covid-19-sitrep-116.pdf?sfvrsn=8dd60956_2
World Health Organization (WHO). New WHO estimates: Up to 190 000 people could die of COVID-19 in Africa if not controlled. Disponível em: https://www.afro.who.int/news/new-who-estimates-190-000-people-could-die-covid-19-africa-if-not-controlled. 07 May 2020.
Further Reading on E-International Relations
- Opinion – How to Call the COVID-19 Pandemic and Why it Matters
- Africa’s COVID-19 Exceptionalism? Same Problems, Different Locations
- Opinion – Lessons America’s Adversaries Can Learn from the Covid-19 Pandemic
- The COVID-19 Pandemic and Climate Change: Why Have Responses Been So Different?
- Putin’s Power Grab Amidst the COVID-19 Pandemic
- The Need for Teachers to Address Racism During the COVID-19 Pandemic