Ebola virus disease (EVD, or Ebola) is a horrifying disease. It seemingly appears out of nowhere, kills people in a gruesome manner, and then disappears for reasons that are not entirely clear. Since Ebola was first described in 1976, it has captured the public imagination and raised questions about how the international community should respond to outbreaks. [1]
West Africa is currently experiencing the largest outbreak of Ebola ever recorded. As of 17 July 2014, the World Health Organisation (WHO) had identified 1048 cases of the disease in Guinea, Liberia, and Sierra Leone since the epidemic began in February. Of those cases, 632 people have died from the disease—a 60 percent case fatality rate. While Ebola’s spread may be slowing in Guinea, Liberia and Sierra Leone recorded 67 new cases and 19 deaths between the 15th and the 17th of July alone. [2] Adding to the tragedy, Sierra Leone’s top Ebola doctor, Sheik Umar Khan, contracted the disease himself. [3]
Stopping the spread of Ebola necessarily requires cross-border cooperation. The disease does not respect national boundaries, and it has already demonstrated a proclivity for spreading to neighboring states. Furthermore, none of the affected states have health care systems or laboratory facilities that can mount an effective response on their own. The international community has an interest in mounting a coordinated response and preventing the epidemic from spreading any further.
Is the current Ebola outbreak in West Africa likely to enhance cooperation among Guinea, Liberia, and Sierra Leone? While it does present opportunities for cooperation, the response has been far from robust so far. There has been a fair amount of discussion about the need to cooperate and provide more resources, but the tangible outcome of these discussions remains lacking. Furthermore, some of the policies that the governments of Guinea, Liberia, and Sierra Leone have introduced in response to the outbreak actually work against effectively containing the disease or building cooperative ties among the countries, like closing borders or threatening to arrest those infected with Ebola. This is not to say that the situation is hopeless, but it does highlight the need to improve cooperative structures among the affected countries.
The Epidemiology of Ebola
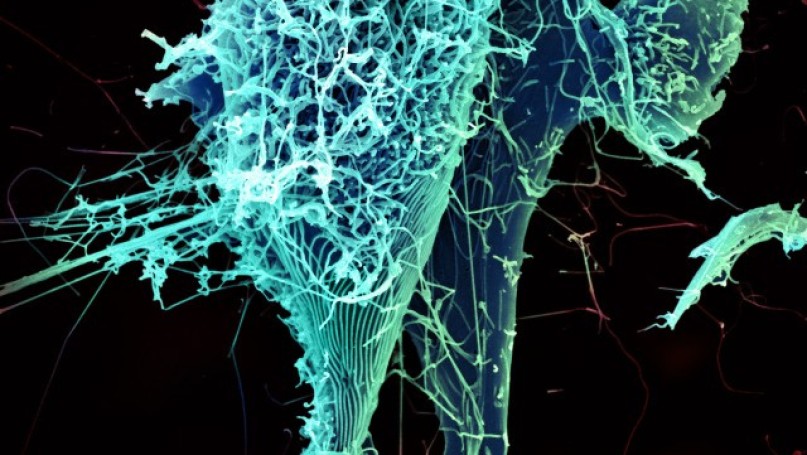
Ebola is a difficult disease to contain under the best of circumstances. Its origins remain uncertain; it appears to spread to humans from animals, though the exact animal reservoir for the disease is not definitively known. Once it enters a human population, Ebola spreads from person-to-person through contact with blood or other bodily fluids. Within 2 to 21 days of infection, symptoms like fever, weakness, and muscle pain appear. From there, the infection progresses to vomiting, bleeding, diarrhea, and eventually multiple organ failure. There exist no treatments or cures for Ebola, so health care workers can only attempt to manage symptoms as they appear. Upwards of 90 percent of those infected die from the disease. [4]
Ebola is particularly insidious because of how it is transmitted. Because it spreads through contact with bodily fluids, health care workers are particularly at risk of contracting the disease as they try to treat patients that come to their clinics. [5] This relationship between health clinics and Ebola’s spread makes people reluctant to seek medical attention, which puts family members at risk of infection. In addition, funeral and burial rites frequently involve close contact between the deceased and family members preparing the body. This sort of close contact with the deceased can increase the likelihood of transmission, because the body’s viral load is at its highest immediately following death. [6] Thus, the very process of mourning the loss of a friend or family member can lead to new cases of Ebola.
Ending an outbreak requires isolating the infected and communicating with local populations about the precautions necessary to prevent infection. This can prove particularly difficult for outsiders who come into Ebola-infected areas, as they rarely possess an understanding of local practices or cultural contexts. [7] Unilaterally banning traditional funeral practices, for example, breeds mistrust and suspicion. A study by Hewlett and Amola about an outbreak of Ebola in Uganda, though, shows that local practices can often be harnessed effectively to reduce the disease’s spread if and when health care workers engage them. [8] Once there have been no new Ebola infections for 42 days, experts declare that an outbreak has officially ended. [9]
Outbreak Timeline
The first suspected cases of Ebola in West Africa appeared in Guinea in February 2014. The cases were centered around Nzerekore, a southern region of the country that borders Sierra Leone, Liberia, and Cote d’Ivoire. [10] By the time Guinea’s Ministry of Health officially reported its Ebola outbreak to the World Health Organisation in March, it had confirmed 49 cases and 29 deaths in four of Guinea’s eight regions. It had identified three suspected cases in the capital city of Conakry—the first time Ebola had ever been seen in a national capital. [11] There were also unconfirmed reports of cases in border regions of Liberia and Sierra Leone when Guinea made its initial report.
After Guinea’s initial report, the disease spread quickly. The Liberian Ministry of Health reported to WHO that it had confirmed its first two cases of Ebola one week later. [12] By 1 April, Guinea had 122 cases of Ebola (24 laboratory confirmed, 98 suspected or probable) and 80 deaths, Liberia had 8 cases and 2 deaths, and Sierra Leone was on alert after the bodies of two people suspected of dying of Ebola in Guinea were brought into the country for burial. [13] Sierra Leone reported its first official Ebola cases on 27 May 2014, identifying 16 cases and 5 deaths. By that point, there were 308 cases among the three states and 200 deaths.
In May, it started to look like the outbreak was slowing down. The rates of new cases and deaths were slowing down, and there was some hope that control measures were showing their efficacy. Unfortunately, the numbers of new cases and deaths spiked in June, fueling speculation that control measures had ended too quickly. [14] The cumulative number of cases crossed 800 and deaths surpassed 500 in early July. By the middle of the month, official figures reported 1048 cases of Ebola (745 of which had been officially confirmed through laboratory tests) and 632 deaths in Guinea (410 cases, 310 deaths), Liberia (196 cases, 116 deaths), and Sierra Leone (442 cases, 368 deaths). [15]
Responding to Ebola
All three affected countries recognise the seriousness of the Ebola outbreak, and they have taken actions in accordance with their international obligations. They have reported their outbreaks to the World Health Organisation and remained in regular contact with the organisation, as required by the International Health Regulations whenever governments detect human cases of Ebola. Officials from the three countries have activated their national infectious disease emergency committees and met with each other to discuss how they can work together. [16]
The international community has also taken steps to supplement the actions of the three governments. The Economic Community of West Africa (ECOWAS) created a ‘solidarity fund’ to contain and manage the outbreak, [17] and the World Health Organisation convened an emergency meeting of regional health ministers in Accra to strengthen surveillance operations and facilitate cross-border consultations. [18] The World Health Organisation also opened a Sub-Regional Outbreak Coordinating Center in Conakry. [19] Doctors Without Borders has deployed 300 personnel to assist in health care facilities, and both the US Centers for Disease Control and Prevention and the European Union have provided scientific personnel and resources to assist with laboratory testing and government coordination. [20]
These are all seemingly positive steps that could contribute to stopping Ebola’s spread; indeed, it is hard to find anything necessarily wrong with them. The problems that arise, though, are threefold. First, many of the responses have been rather tardy. The World Health Organisation fulfilled its coordinating mission by organising a meeting of regional health officials in Accra in early July—but that was three-and-a-half months after the first report of the disease. WHO’s Sub-Regional Outbreak Coordination Center has the potential to be a useful resource, but it took nearly four months from the outbreak’s beginning until WHO began such operations. Given how quickly Ebola spreads and its virulence, such a delay helped the disease gain a foothold in the region. Arresting the spread of infectious diseases requires quicker action.
Second, financial resources for addressing Ebola containment remain lacking. The governments of Guinea, Liberia, and Sierra Leone cannot afford to increase their health spending to address the Ebola outbreak. Liberia and Sierra Leone already have the two highest total expenditures on health as percentage of GDP in the world. [21] The health care systems of both countries were also devastated by recent civil wars, and Guinea’s under-resourced health care system faced additional burdens due to the influx of refugees from Liberia and Sierra Leone. [22] Even if these governments wanted to pool their resources to build laboratory, surveillance, or health care services, they simply lack the ability to do so. All of this means that regional governments will need to look to outsiders to finance an effective response to Ebola in the short-term. Health care workers wear bulky, protective suits in an effort to avoid infection, and public handwashing stations with chlorinated water have been established in some cities. Unfortunately, the protective suits are not foolproof, as evidenced by Sheif Umar Khan’s infection, and the price of chlorine has tripled, making it harder to come by. [23] Nurses at the hospital in Kenema, Sierra Leone, went on strike on 21 July to protest the government’s failure to provide them with sufficient protective gear to protect against the disease, and a lack of adequate pay. [24] Kenema is home to Sierra Leone’s only Ebola testing facility and houses the highest number of Ebola patients.
Unfortunately, it is uncertain what sort of financial resources will be available. ECOWAS’ solidarity fund for Ebola reportedly has $3.5 million in contributions, but it is not entirely clear how or when those funds will be distributed to the effected governments. [25] The European Union’s contribution of approximately $675,000 will be useful, but Liberia alone has indicated that it will need at least $1.5 million to combat Ebola. [26] While the World Health Organisation can take a role in coordinating an international response, it lacks the ability to provide much direct financial assistance to the effected countries. The low level of financial resources available for responding to Ebola does not lend itself to facilitating international cooperation among the states facing an Ebola outbreak.
Third, the governments have introduced some policies that actually work against an effective response to Ebola. As noted above, one of the keys to stopping an Ebola outbreak is to isolate the infected (or potentially infected) so that they cannot spread the disease to others. The idea is that isolation will break the chain of transmission. Unfortunately, the governments of Liberia and Sierra Leone have introduced punitive rules that essentially criminalise Ebola. Liberian President Ellen Johnson Sirleaf announced that “anyone found or reported to be holding suspected Ebola cases in homes or prayer houses can be prosecuted,” and Sierra Leone has enacted a similar policy. [27] On the face of it, this sort of policy would help ensure the government knew where Ebola patients were. In practice, though, these sorts of punitive measures can encourage families to hide loved ones and do whatever they can to avoid the health care system. As a result, these people go underground, where the chances that they can spread infection increases. [28] This criminalisation response can also help foster suspicion, conspiracy theories, and violence against health care workers. [29] Other governments in the region have contributed to stigmatising Ebola patients, which can reinforce a desire by patients or their families to hide so as to avoid notice. Sierra Leone closed its border crossings with both Guinea and Liberia, even though WHO specifically advises against taking such measures. [30] Senegal closed its southern border with Guinea for a month, and Mauritania closed its most of its border crossings along the Senegal River—even though Mauritania does not border any of the countries with Ebola cases. [31] It is worth highlighting, though, that government officials in Guinea and Liberia specifically chose to keep their border crossings open in order to facilitate a more robust response to the disease. [32]
Moving Forward
With the number of Ebola cases in West Africa continuing to increase, it is of utmost importance that the affected governments and the international community take concerted actions to try and stop the disease’s spread. Three elements are vital to implementing an effective response.
First, the current response needs to be ratcheted up. Opening sub-regional command centers, deploying personnel from governmental and nongovernmental sources, and providing financial resources are all important—but they need to be done in greater number and with greater urgency. The initial efforts are not necessarily failures; they are just too small and slow in response to the overwhelming nature of this unprecedented outbreak. The meeting of regional health ministers in Accra in mid-July led to an agreement to increase cross-border cooperation, engage local communities better, and foster collaborations with international partners. This may provide a solid foundation for ratcheting up a more aggressive response to the outbreak, though press reports note that the summit’s final communiqué included few details about how these plans would be implemented. [33]
Second, efforts to provide health care services and outreach to affected communities need to take concerted efforts to integrate local cultural contexts and health care measures into Ebola control. Rather than dismissing rumors as evidence of a lack of information, successful health interventions frequently try to tailor their messages in such a way that incorporate the rumors and the shared understandings about health and wellness that they embody. [34] In other words, the problem is less one of ignorance and more one of trying to send a message that fails to resonate. By a similar token, measures that criminalise or stigmatise Ebola patients or those potentially infected with the disease are unlikely to encourage compliance. A more promising strategy is the song “Ebola in Town” by D-12, Shadow, and Kuzzy of 2 Kings [35]—a rap with a “catchy, trippy electro-dance beat” that instructs listeners about the proper steps to take to avoid infection. Using music both gets around issues of illiteracy and reaches audiences who might overlook official government pronouncements. [36]
Third, there need to be serious long-term efforts to improve the health care systems, disease surveillance capabilities, and laboratory resources in all three states. Part of the reason for the delay between the first rumored cases of Ebola in Guinea in February and the official announcement in late March was because laboratory facilities were not available to conduct the necessary tests. Therefore, by the time the Guinean government could get the tests done, nearly 50 people were already infected with Ebola. Undertaking a long-term campaign to strengthen such systems would allow these governments to respond more quickly and have a greater chance of stopping any future outbreak. They would also help build strong ties between these governments and the rest of the international community to further the promotion of health.
Notes
[1] Laurie Garrett, The Coming Plague: Newly Emerging Diseases in a World Out of Balance (New York: Farrar, Straus, and Giroux, 1994).
[2] World Health Organisation, “Ebola virus disease, West Africa—update,” 19 July 2014. http://www.who.int/csr/don/2014_07_19_ebola/en/ (accessed 22 July 2014).
[3] Umaru Fofana, “Sierra Leone’s chief Ebola doctor contracts the virus,” Reuters, 23 July 2014. http://in.reuters.com/article/2014/07/23/us-health-ebola-africa-idINKBN0FS10T20140723 (accessed 23 July 2014).
[4] World Health Organisation, “Ebola virus disease,” http://www.who.int/mediacentre/factsheets/fs103/en/ (accessed 22 July 2014).
[5] Jason Beaubien, “Ebola is a deadly virus—but doctors say it can be beaten,” NPR, 22 July 22, 2014. http://www.npr.org/blogs/goatsandsoda/2014/07/22/333628899/ebola-is-a-deadly-virus-but-doctors-say-it-can-be-beat (accessed 22 July 2014).
[6] Beaubien, “Ebola is a deadly virus”; Paolo Francesconi, Zabulon Yoti, Silvia Declich, Paul Awil Onek, Massimo Fabiani, Joseph Olango, Roberta Andraghetti, Pierre E. Rollins, Cyprian Opira, Donato Greco, and Stefania Salmaso, “Ebola hemorrhagic fever transmission and risk factors of contacts, Uganda,” Emerging Infectious Diseases, Vol. 9, No. 11 (2003), http://wwwnc.cdc.gov/eid/article/9/11/03-0339_article (accessed 22 July 2014); Barry Hewlett and Bonnie Hewlett, Ebola, Culture, and Politics: The Anthropology of an Emerging Disease (New York: Cengage, 2007): 78-79;
[7] Kim Yi Dionne, “Why West African governments are struggling in response to Ebola,” The Monkey Cag, 15 July 2014. http://www.washingtonpost.com/blogs/monkey-cage/wp/2014/07/15/why-west-african-governments-are-struggling-in-response-to-ebola/ (accessed 22 July 2014).
[8] Barry Hewlett and Richard P. Amola, “Cultural contexts of Ebola in northern Uganda,” Emerging Infectious Diseases, Vol. 9, No. 10 (2003), http://wwwnc.cdc.gov/eid/article/9/10/02-0493_article (accessed 22 July 2014).
[9] Centers for Disease Control and Prevention, “Ebola hemorrhagic fever,” 21 July 2014. http://www.cdc.gov/vhf/ebola/resources/outbreaks.html (accessed 22 July 2014).
[10] BBC News, “Ebola outbreak in Guinea unprecedented—MSF,” 31 March 2014. http://www.bbc.com/news/world-africa-26825869 (accessed 22 July 2014).
[11] World Health Organisation Regional Office for Africa, “Ebola viral disease in Guinea,” 23 March 2014. http://www.afro.who.int/en/clusters-a-programmes/dpc/epidemic-a-pandemic-alert-and-response/outbreak-news/4063-ebola-hemorrhagic-fever-in-guinea.html (accessed 22 July 2014).
[12] World Health Organisation, “Ebola virus disease in Liberia,” 30 March 2014. http://www.who.int/csr/don/2014_03_30_ebola_lbr/en/ (accessed 22 July 2014).
[13] World health Organisation, “Ebola virus disease, West Africa,” 1 April 2014. http://www.who.int/csr/don/2014_04_01_ebola/en/ (accessed 22 July 2014).
[14] Terrence McCoy, “This is now the deadliest Ebola outbreak on record—and it’s getting worse,” Washington Post, 27 June 2014. http://www.washingtonpost.com/news/morning-mix/wp/2014/06/27/this-is-now-the-deadliest-ebola-outbreak-on-record-and-its-getting-worse/ (accessed 22 July 2014).
[15] Centers for Disease Control and Prevention, “Outbreak of Ebola in Guinea,” 2 July 2014. http://www.cdc.gov/vhf/ebola/outbreaks/guinea/ (accessed 22 July 2014).
[16] World Health Organisation Regional Office for Africa, “Ebola virus disease, Guinea (situation as of 30 March 2014),” 30 March 2014. http://www.afro.who.int/en/clusters-a-programmes/dpc/epidemic-a-pandemic-alert-and-response/outbreak-news/4071-ebola-haemorrhagic-fever-guinea-30-march-2014.html (accessed 22 July 2014).
[17] Voice of Nigeria, “ECOWAS establishes Ebola solidarity fund,” 12 July 2014. http://www.voiceofnigeria.org/index.php/africa/item/2029-ecowas-establishes-ebola-solidarity-fund (accessed 22 July 2014).
[18] World Health Organisation Regional Office for Africa, “Special Ministerial Meeting on Ebola Virus Disease in West Africa, Accra, Ghana, 2-3 July 2014,” http://www.afro.who.int/en/clusters-a-programmes/dpc/epidemic-a-pandemic-alert-and-response/epr-highlights/4187-special-ministerial-meeting-ebola-accra-2-3-july-2014.html (accessed 22 July 2014).
[19] World Health Organisation, “Ebola virus disease, West Africa,” 15 July 2014. http://www.who.int/csr/don/2014_07_15_ebola/en/ (accessed 22 July 2014).
[20] European Union, “Ebola in West Africa: European Union joins efforts to stop spread of disease and releases €500,000 in immediate funding,” 28 March 2014. http://europa.eu/rapid/press-release_IP-14-345_en.htm (accessed 22 July 2014).
[21] Central Intelligence Agency, “Country Comparisons: Health Expenditures.” https://www.cia.gov/library/publications/the-world-factbook/rankorder/2225rank.html?countryname=Liberia&countrycode=li®ionCode=afr&rank=1#li (accessed 22 July 2014).
[22] Kim Yi Dionne, “Why West African governments.”
[23] Umaru Fofana, “How to ignore a plague,” Medium, 11 July 2014. https://medium.com/matter/how-to-ignore-a-plague-14ea08694cc (accessed 24 July 2014).
[24] Umaru Fofana, “Sierra Leone religious leaders criticize government handling of Ebola,” Reuters, 21 July 2014. http://www.reuters.com/article/2014/07/21/us-health-ebola-africa-idUSKBN0FQ0XO20140721 (accessed 24 July 2014).
[25] Voice of Nigeria, “ECOWAS establishes Ebola solidarity fund,” 12 July 2014. http://www.voiceofnigeria.org/index.php/africa/item/2029-ecowas-establishes-ebola-solidarity-fund (accessed 22 July 2014).
[26] E.J. Nathaniel Daygbor, “Health Ministry wants US$1.5m to fight Ebola,” New Dawn, 11 July 2014. http://www.thenewdawnliberia.com/index.php?option=com_content&view=article&id=12115:health-ministry-wants-us15m-to-fight-ebola&catid=46:health&Itemid=60 (accessed 22 July 2014).
[27] Krista Larson, “Ebola crisis in West Africa deepens; 500+ dead,” Associated Press, 14 July 2014. http://hosted2.ap.org/APDEFAULT/3d281c11a96b4ad082fe88aa0db04305/Article_2014-07-14-AF–West%20Africa-Ebola/id-c1e0d69c76a441449605ad2ae9b4d97a (accessed 22 July 2014).
[28] Eugenia Tognotti, “Lessons from the history of quarantine, from plague to influenza A,” Emerging Infectious Diseases, Vol. 19, No. 2 (2013): 254-259.
[29] Fofana, “How to ignore a plague.”
[30] Reuters, “Sierra Leone shuts borders, closes schools to fight Ebola,” 11 June 2014. http://uk.reuters.com/article/2014/06/11/us-health-ebola-leone-idUKKBN0EM2CG20140611 (accessed 23 July 2014).
[31] Saliou Samb, “Deadly Ebola virus spreads from rural Guinea to capital,” Reuters, 28 March 2014. http://in.reuters.com/article/2014/03/27/guinea-ebola-idINDEEA2Q0JX20140327 (accessed 23 July 2014).
[32] C.Y. Kwanue, “Guinean gov’t provides Ebola update,” The Liberian Observer, 4 July 2014. http://www.liberianobserver.com/news/guinean-gov’t-provides-ebola-updates (accessed 23 July 2014).
[33] Al Jazeera English, “West Africa states adopt new Ebola strategy,” 11 July 2014. http://www.aljazeera.com/news/africa/2014/07/west-africa-states-adopt-new-ebola-strategy-201473233256968685.html (accessed 23 July 2014).
[34] Amy Kaler, “Health interventions and the persistence of rumor: the circulation of sterility stories in African public health campaigns,” Social Science and Medicine, Vol. 68, No. 9 (2009): 1711-1719.
[35] “Ebola in Town,” https://soundcloud.com/shadowmrgn/ebola-in-town-d-12-shadow-kuzzy-of-2kings (accessed 23 July 2014).
[36] Monica Mark, “Ebola virus causes outbreak of infectious dance tune,” The Guardian, 27 May 2014. http://www.theguardian.com/world/2014/may/27/ebola-virus-outbreak-infectious-dance-tune (accessed 23 July 2014).
Further Reading on E-International Relations
- Chaos and Corruption in West Africa: Lessons from Sierra Leone
- American Global Health Internationalism and the Ebola Crisis in West Africa
- Ebola Response in the Democratic Republic of Congo: A Bridge to Peace?
- Adding Fuel to the Fire? American Security Cooperation in Sub-Saharan Africa
- What International Relations Tells Us about COVID-19
- The COVID-19 Outbreak: A Testing Time for NGOs in Bangladesh